The healthcare supply chain has experienced several lifetimes of learning in the last three years. We’ve faced one black swan event after another: pandemics, port delays, record inflation, and spot shortages of critical goods. And as soon as one set of disruptions eases, other challenges emerge to take their place: threats of railroad strikes, diesel fuel shortages, new COVID outbreaks in China, and other threats to the supply chain.
Anyone looking for a “return to normal” following COVID-19 is sure to be disappointed. Supply chain disruptions aren’t going away. Prior to the pandemic, the top priorities for most healthcare supply chain leaders were efficiency and cost control. The pandemic changed that — suddenly, resilience overshadowed other concerns. Efficiency and resilience are generally viewed as trade-offs; in that more of one means less of the other. But this is a false choice.
The feature stories in this issue are devoted to examining how to navigate the “new normal” in the medical supply chain. We will review research that demonstrates how providers have changed their priorities with respect to supply chain management. We provide an update on HIDA’s legislative efforts to expedite medical supplies through our nation’s ports. Another article introduces a new online dashboard HIDA developed in partnership with the federal government that helps providers manage stockpiles and supply chain disruptions during pandemics and natural disasters.
New Supply Chain Realities Prompt Distributors To Embrace New Solutions
The COVID-19 pandemic made a profound change on role of the supply chain manager — with regards to the centrality of the role to hospital operations as well as the expectations of the role. These issues were the subject of a Thought Leaders roundtable discussion at the recent joint meeting of the HIDA and HIDA Educational Foundation Boards of Directors. Participants heard from Nicholas Hula, a research consultant for Advisory Board, who shared his findings in a presentation titled The New Health Care Supply Chain Mandate.
More Widespread Shortages
About 93% of provider executives report they are still experiencing product shortages. Not only are the shortages more widespread, but they also have become more difficult to anticipate. In 2020, providers scrambled for items like masks, testing, supplies, disinfectants, and ventilators. Now that list of potential shortages has grown exponentially.
Growing Unpredictability
Every link in the supply chain is potentially fragile. Manufacturers rely on a handful of global sources for raw materials such as resins and aluminum. Key component parts are sourced from a limited set of vendors. When manufacturers centralize production to gain economies of scale, it often makes the supply chain geographically vulnerable to external shocks.
Shifting Provider Priorities
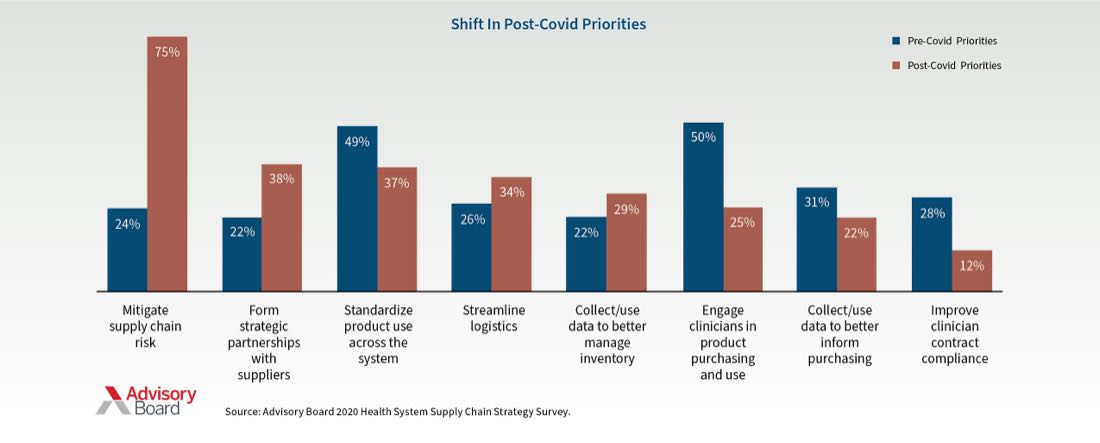
Before COVID, the top three supply chain priorities for providers were engaging clinicians in product purchasing and use (50%), standardizing product use across the system (49%), and data collection (31%). Post-COVID, the top priorities are mitigating supply chain risk (75%), forming strategic partnerships with suppliers (38%), and streamlining logistics (34%).
 Best Practices And Solutions
Best Practices And Solutions
These findings prompted a wide-ranging discussion on best practices and solutions. For many of the issues providers are facing, distributors can be trusted partners to collaborate on solutions.
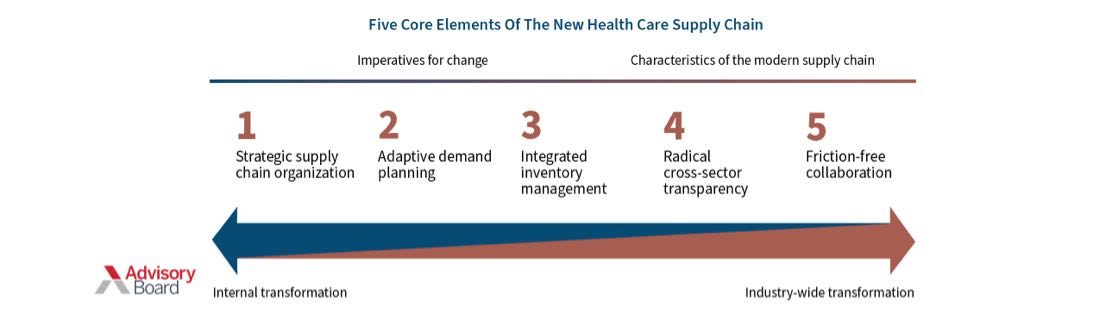
Engage Strategically
Providers are under enormous financial pressure, and supply chain can be a financial differentiator. Distributors can broaden their reach into health systems by engaging with a variety of executives — such as chief nursing officers and chief medical officers.
Plan Proactively
The pandemic highlighted the need for improved demand forecasting for medical products. Demand planning needs to be more proactive and future focused and less dependent on old algorithms and historical data that the pandemic has rendered obsolete.
Integrate Inventory Management
Traditional inventory management improvement initiatives tend to be isolated and focus on single departments or service lines. Such isolation costs money in the long run because it becomes easier for providers to purchase more product than to consider ways to better manage their existing inventory. Distributors can help providers take a more holistic approach to inventory management.
Redefine Visibility And Transparency
Health system leaders lack access to accurate, real-time data on supply availability and use. This leads to an increased risk of expired products and redundant purchasing. Improvements in visibility — both upstream and downstream in the supply chain — can unlock opportunities to reduce waste and increase flexibility. This requires strong commitments with distributors to share data among trusted trading partners.
Collaborate Freely
When clinicians are concerned that they won’t have access to necessary supplies, they can undermine supply chain management by creating their own “secret stashes” of products. It is essential for managers to build trust among clinicians to eliminate hoarding. Integrate product demand planning with clinical planning to optimize purchasing and product use.
Fast Pass Legislation Remains Key Priority For 2023

Supply chain friction is here to stay, in one form or another. As one set of disruptions has eased, other challenges have emerged in their place. The persistence of supply chain issues make it essential for Congress to create a “fast pass” channel for medical supplies through U.S. ports.
During the extreme shipping bottlenecks that occurred in the last six months of 2021, HIDA worked diligently to find solutions to expedite medical supplies to providers and patients who needed them. HIDA urged the White House Supply Chain Disruptions Task Force to prioritize critical medical supplies. By partnering with port officials, terminal operator SSA Marine, and port technology provider eModal, HIDA was able to implement a fast pass pilot program at the Ports of Los Angeles and Long Beach.
The Biden administration recognized the success of these ad-hoc cargo initiatives. In its February 2022 report Supply Chain Assessment of the Transportation Industrial Base, the U.S. Department of Transportation identified one of the key successes to resolving the 2021 supply chain congestion was “developing a fast pass system to expedite global transportation of essential medical products.”
HIDA has spent the past year working with ports, federal officials, and Members of Congress to turn the temporary use of fast pass during the pandemic into an ongoing transportation solution. To that end, HIDA has been working with bipartisan Members of Congress on the House Transportation and Infrastructure Committee to draft legislative language for the creation of a Fast Pass Critical Cargo Pilot Program for Medical Supplies.
Such a pilot program would authorize the Secretary of Transportation (in coordination with the Secretary of Health and Human Services and the Secretary of Homeland Security) to partner with one or more marine terminal operators to develop a process to identify critical cargo and expedite movement through the ports.
The persistence of supply chain issues
make it essential for Congress to create a “fast pass”
channel for medical supplies through U.S. ports.